How sleep affects health is more far-reaching than most people realize. New science reveals it impacts not just your brain and energy, but pain levels, mood, and even chronic conditions like arthritis and fibromyalgia. So, if you’ve ever wondered why a few bad nights leave you exhausted, foggy, or in pain, this research explains why — and how to fix it.
New science shows how sleep affects health in surprising ways. Sleep powers your heart, brain, gut, and immune system. It boosts muscle recovery, sharpens mental clarity, and balances emotions. However, poor sleep does more than exhaust you. It disrupts vital systems, accelerates brain aging, and triggers flare-ups of chronic conditions like arthritis, fibromyalgia, and chronic fatigue.
This article explores the latest science on how sleep impacts health, from the adult brain to children’s brain development and focus. It covers the body’s holistic systems, including the gut’s link to serotonin and melatonin. You’ll learn how to optimize sleep with the Anti-Inflammatory Rainbow Diet™ and more.
I know sleep deprivation’s devastating effects firsthand. When I was a practicing CPA, getting enough sleep during tax season was tough. Years of stress and poor sleep wrecked my gut and health, causing widespread muscle pain. Fortunately, I manage my fibromyalgia and irritable bowel syndrome (IBS) well now.
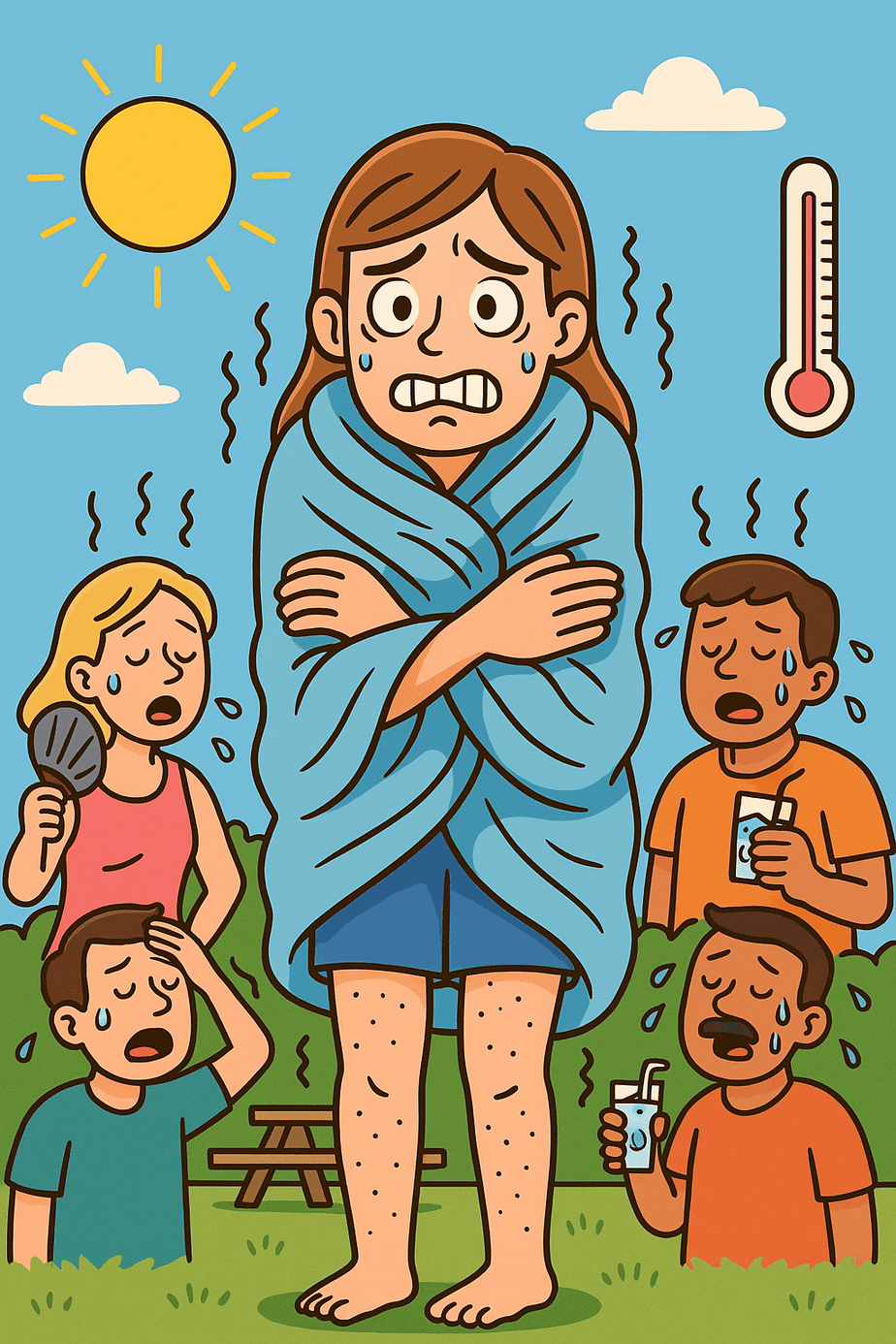
However, even now, two or three sleepless nights can trigger flares. Additionally, poor sleep brings chilling goosebumps, even in hot weather, as if I’m cold. If you notice pain or “mystery” symptoms after poor sleep, you’re not alone. Science explains how sleep affects health—and offers solutions.
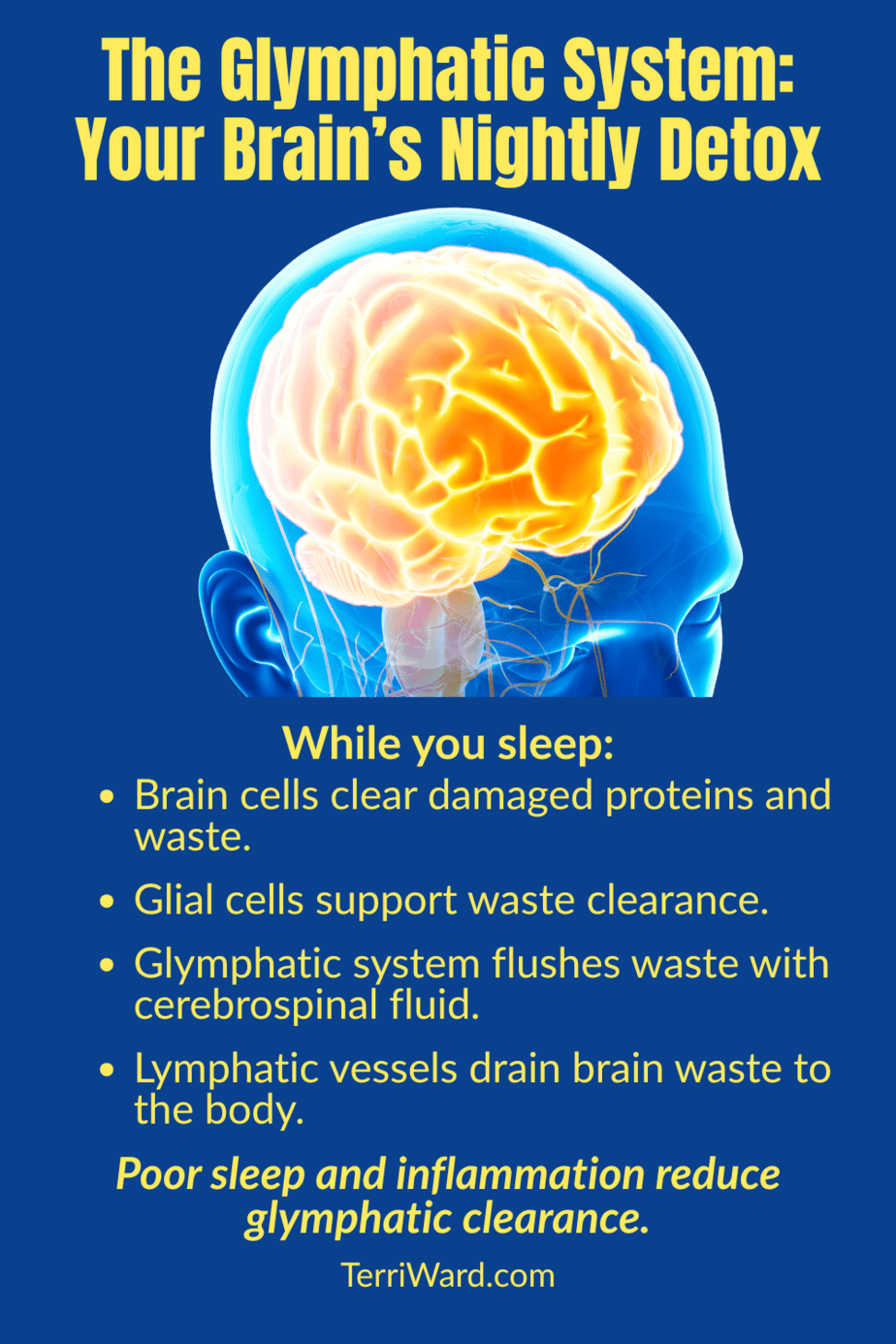
How Sleep Detoxes Your Brain and Protects Memory
Did you know that during sleep your brain performs its most important maintenance work? Sleep powers health by cleansing your brain. During deep sleep, the glymphatic system flushes out waste, including toxic proteins like amyloid plaques, which are linked to Alzheimer’s disease.
Impaired toxin clearance: A 2025 study found that poor sleep hinders this clearance process. As a result, toxins build up in the brain, raising risks for memory loss and dementia and accelerating brain aging.
Dementia risk increase: Similarly, a 2021 study linked getting less than six hours of sleep each night to a 30% higher risk of developing dementia. For children, poor sleep also impairs focus and brain development.
Silent brain injuries: Additionally, a 2024 study showed that getting less than 7 or more than 9 hours of sleep causes silent brain injuries. These injuries can foreshadow stroke and dementia later in life.
Why Sleep Medications May Not Be the Best Solution
Popular sleep aids such as benzodiazepines (like Xanax) and antihistamines (like Benadryl) may help you fall asleep. However, they can reduce restorative deep and REM sleep — the very stages your brain needs. Long‑term use of these medications is linked to higher dementia risk.
In contrast, melatonin, is unique. It’s a natural hormone and antioxidant that helps protect brain cells. However, it’s best used in small doses, for short periods, and ideally only after addressing root causes (more on that in the gut‑sleep section).
Why Some People Feel Cold in Heat After Sleep Loss
When I get goosebumps in 90‑degree heat after a bad night’s sleep, it’s because poor sleep can disrupt thermoregulation— your body’s ability to control temperature. The hypothalamus, a part of the brain, normally keeps this in balance. When it’s thrown off, your body can misread temperature signals, leaving you feeling chilly when you shouldn’t be.
This reflects a wider issue: sleep loss stresses your autonomic nervous system, which is the control center for automatic functions like heart rate, digestion, and stress responses. This explains why sleep problems can trigger strange and seemingly unrelated symptoms.
Note: Persistent cold sensitivity can also occur with hypothyroidism, which slows metabolism and reduces heat production. If you suspect thyroid issues, seek out a practitioner experienced in internal or functional medicine for a thorough evaluation. Most primary care practitioners will only order a TSH test, which does not give a complete picture. A full thyroid panel, including free T4, free T3, reverse T3, and thyroid antibodies is necessary.
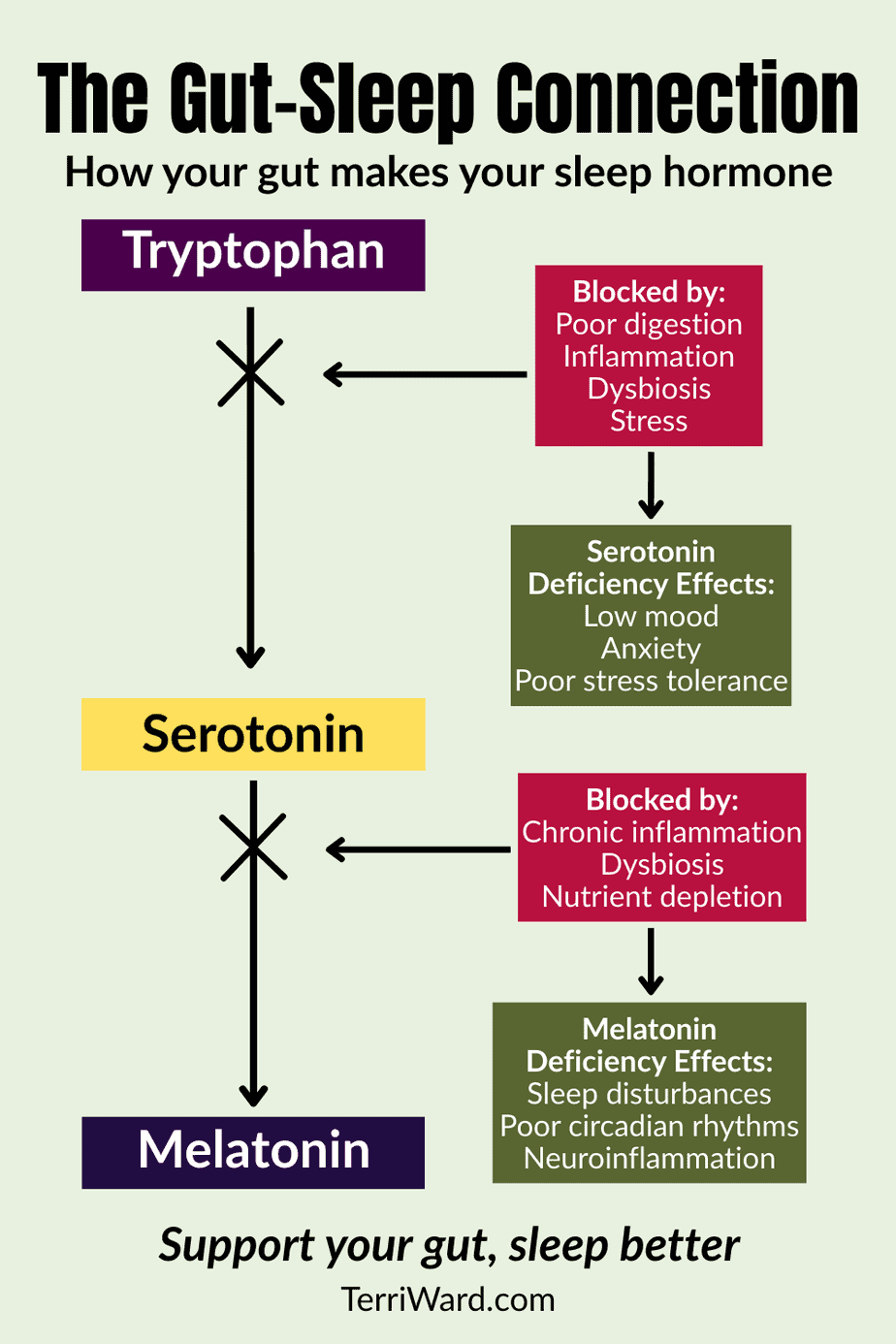
The Gut–Sleep Connection: Serotonin, Melatonin & Mood
Your gut makes about 90% of your serotonin — the brain’s “feel-good” chemical that boosts mood and helps control sleep. Serotonin is the raw ingredient your body uses to make melatonin, the hormone that signals when it’s time to sleep. It also helps regulate the release of dopamine, which boosts motivation and focus. Disruptions in this regulation may contribute to conditions like depression, anxiety, and attention disorders.
If your gut isn’t healthy due to poor diet, inflammation, or imbalanced gut bacteria (dysbiosis), serotonin production drops. With less serotonin, your body produces less melatonin, and sleep quality suffers. I know this all too well — when I lose sleep, my IBS flares because:
-
- First, sleep loss increases gut inflammation and intestinal permeability (“leaky gut”).
- Second, it disrupts the balance of healthy bacteria, reducing serotonin output.
- Third, the resulting melatonin drop makes nighttime rest even harder, creating a vicious cycle.
Improving gut health can reverse this. Studies show that eating more fiber, adding probiotics, and reducing inflammation can boost serotonin naturally and promote healthy sleep patterns.
This underlines why melatonin supplements should come after addressing gut health, not as a first-line or long-term fix. Without fixing the gut, supplements may mask deeper problems, and long‑term use can interfere with your body’s own hormone balance.
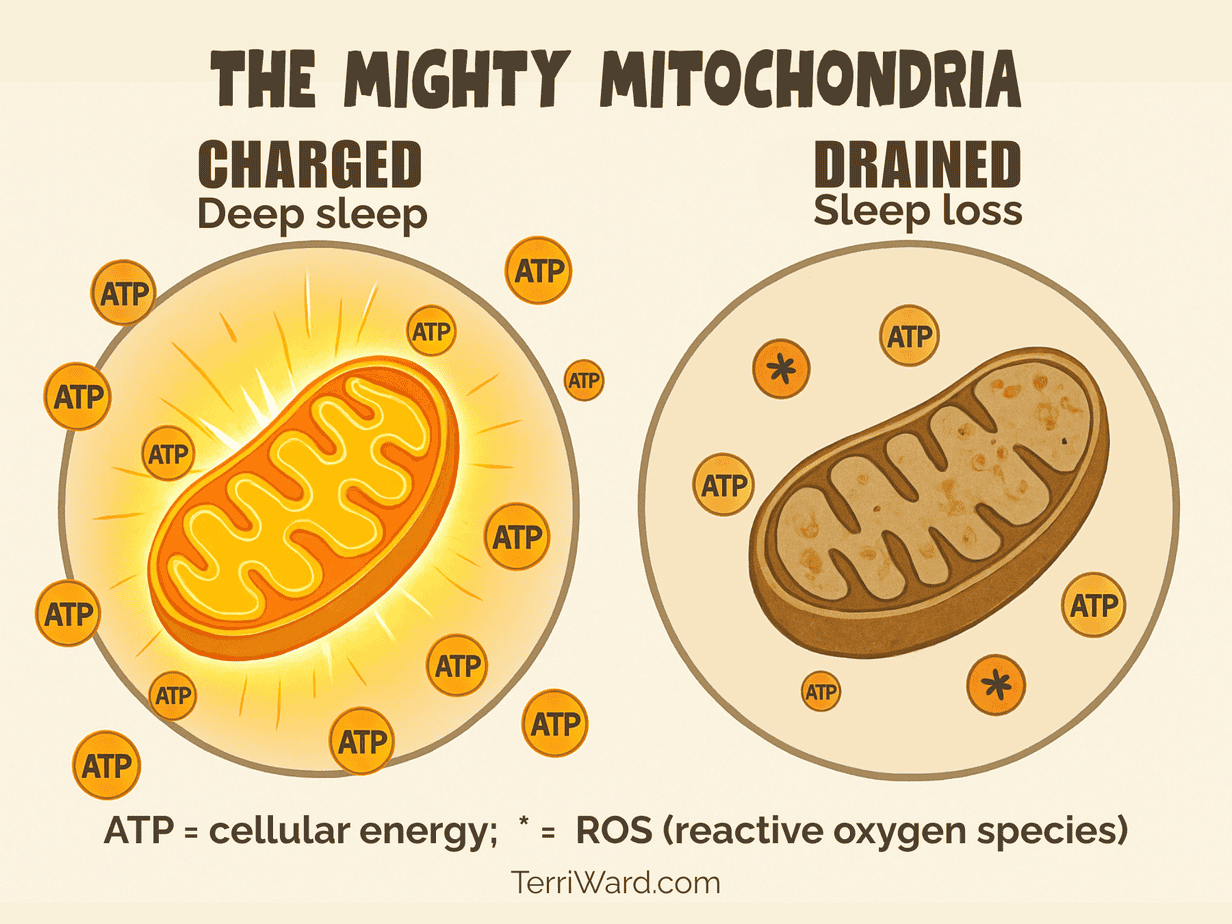
Boosting Energy & Easing Pain: Sleep’s Impact on Mitochondria
Mitochondria power your cells. These tiny “batteries” produce energy in the form of adenosine triphosphate (ATP) that our muscles, nerves, and organs can use. When mitochondria thrive, you feel energized, experience less pain, and gain sharper focus. However, poor sleep disrupts how sleep affects health through mitochondria, triggering oxidative stress and inflammation.
Oxidative stress happens when harmful molecules called free radicals — also known as reactive oxygen species (ROS) — overwhelm your body’s defenses, known as antioxidants. Sufficient antioxidants from fruits and vegetables help neutralize these molecules before they can do harm. Otherwise, when free radicals build up, they damage cells much like rust eats away at metal, draining energy and increasing pain.
In turn, this cell damage triggers inflammation, which can worsen chronic conditions like fibromyalgia, arthritis, and chronic fatigue. It can also harm nerve cells, speeding up brain aging and raising the risk of neurodegenerative diseases.
Poor sleep makes this worse by:
-
- Increasing oxidative stress that harms mitochondria.
- Limiting deep sleep, where repair and recovery occur.
- Altering hormones, such as growth hormone, which support mitochondrial health.
Consequently, sleepless nights do more than exhaust you. They drain energy, heighten pain, and cloud thinking. In kids, this impairs growth and focus. For adults, it can trigger fibromyalgia or arthritis flare-ups. By improving sleep, you reduce oxidative stress and enhance how sleep affects health overall.
How Sleep Affects Health for Kids and Their Brain Development
For children and teens, getting enough sleep is essential for brain and body growth, learning and memory, emotional balance, and a strong immune system. Yet about one-third struggle with insomnia or poor sleep quality. In response, some parents may turn to doctors who prescribe drugs like Ritalin or antidepressants. However, these miss addressing root causes such as irregular bedtimes, screen use, poor diet, or gut health.
Without tackling these underlying factors, children continue to miss out on the restorative rest crucial for their overall health and well-being.
When young people get less sleep — for example, dropping from about 10 hours to 7 hours a night — their ability to pay attention and remember information declines. Thinking becomes less flexible, reaction times slow, and school performance suffers. A 2025 study found that this kind of sleep loss caused more than a 20% drop in memory and concentration, along with lower test scores. Mood also takes a hit, with more irritability, sadness, anger, and fatigue, and less energy or motivation.
Scientists believe these changes happen because sleep loss alters brain activity, including in the amygdala, which helps control emotions. This can make feelings harder to manage and increase emotional ups and downs. It also weakens the brain’s network connections for decision-making and self-control, making it harder to focus and think clearly. Irregular bedtimes and late‑night screen use make these issues even worse and can set patterns that persist into adulthood.
Poor sleep also affects the body. It disrupts hunger hormones, raising levels of ghrelin, which increases appetite, and makes high‑calorie, less healthy foods more tempting.
Over time, this can cause insulin resistance, weight gain, and a higher risk for type 2 diabetes. Teens who don’t sleep well are also more likely to take risks, have trouble controlling impulses, and develop mental health challenges like anxiety and depression.
Sleep-Boosting Steps for Kids
Simple steps like the following can make a big difference for their learning, mood, and long-term health:
- Consistent bedtime and wake time, even on weekends.
- Dimming lights and stopping screen use an hour before bed.
- Nutrient-rich diet with sufficient magnesium and vitamin D.
- Gentle natural approaches first, such as tart cherry juice, before turning to anti-depressants, melatonin, or medication.
Regular, high-quality sleep is one of the best ways to help young people grow strong, think clearly, and stay emotionally balanced.
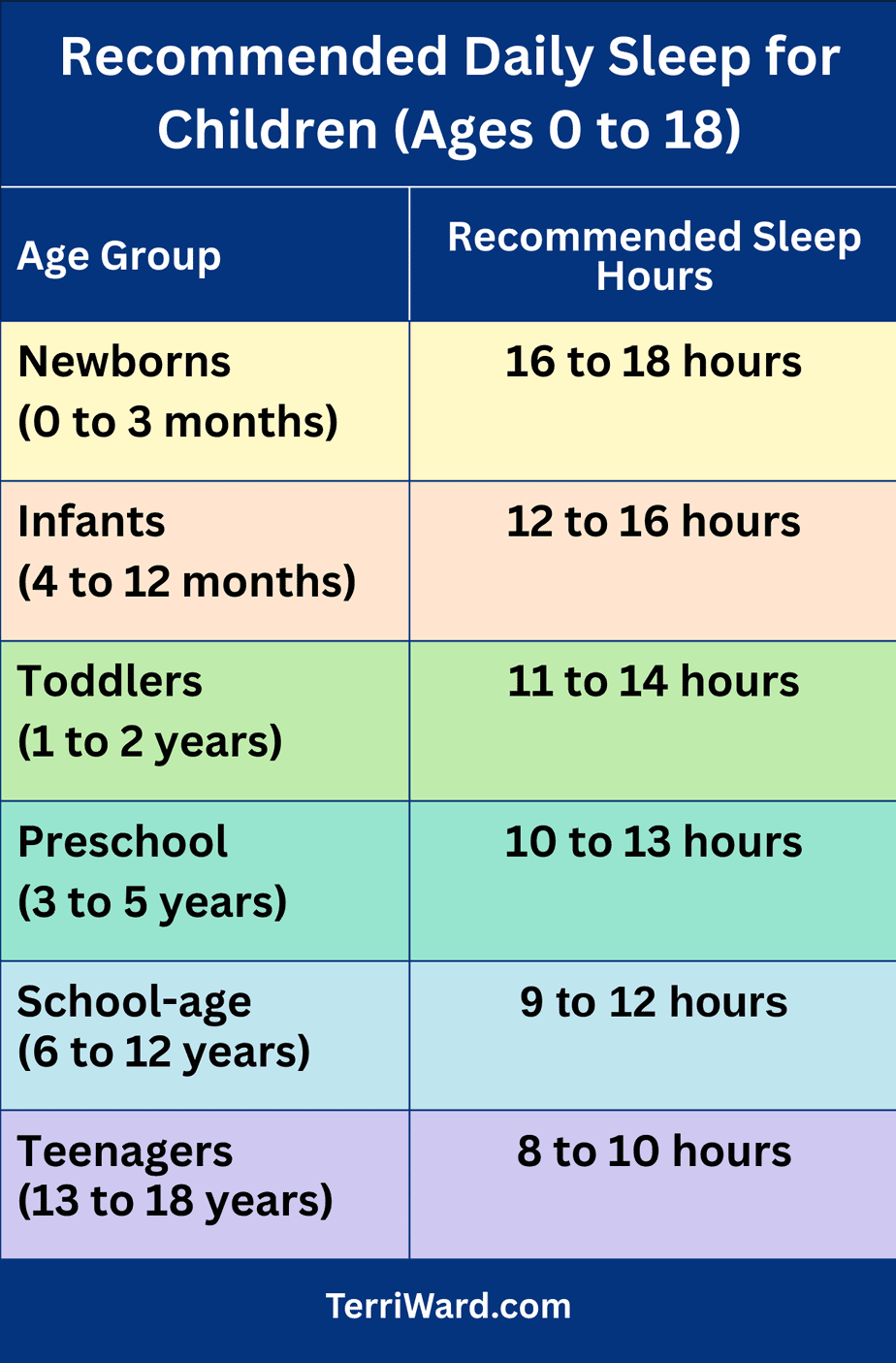
Recommended Sleep Hours for Children and Teens
The accompanying table summarizes general guidelines for total daily sleep time (including naps) for children by age, based on recommendations from the American Academy of Sleep Medicine. It’s important to remember that each child is unique and may have different sleep needs. I recall my mother being frustrated that I didn’t need as much sleep as my older sister, but these recommended ranges are designed to accommodate such individual differences.
For more detailed guidelines, visit the American Academy of Sleep Medicine’s Pediatric Sleep Recommendations or the Sleep Foundation’s Children and Sleep page.
The Whole‑Body Toll of Poor Sleep
Sleep deprivation affects far more than your brain and gut health. It sets off a ripple effect through nearly every system in the body, creating problems that can add up over time.
One of the first areas to suffer is your immune system. Without enough restorative rest, your body produces fewer infection‑fighting proteins, such as cytokines, and the healing process slows down. As a result, you’re more likely to catch illnesses and may take longer to recover when you do get sick.
Your metabolism also feels the impact. Poor sleep disrupts the balance of hunger hormones, increasing ghrelin levels that boost appetite and making calorie‑dense foods more appealing. If this pattern continues, it can lead to insulin resistance — a key factor in weight gain and a higher risk of type 2 diabetes.
The heart and circulatory system aren’t spared either. When you’re short on sleep, stress hormones like cortisol rise, which can elevate blood pressure and put extra strain on your heart. Over time, this added stress may increase your chances of developing cardiovascular problems, especially if you already have other risk factors.
Even your muscles and connective tissues need quality sleep. This is when much of the body’s repair work happens, so missing out on deep rest can slow recovery after exercise or injury.
Solutions to Enhance How Sleep Affects Health
Better sleep transforms your health. For example, you can boost how sleep affects health with simple habits like these:
- Set a sleep schedule. Go to bed and wake up at the same time daily. This regulates hormones and supports cellular repair.
- Keep your bedroom cool and dark. A temperature of 65–68°F is ideal. Darkness boosts melatonin for better rest. Use room-darkening window coverings or an eye mask.
- Get morning sunlight soon after waking. Natural light early in the day resets your body’s internal clock and supports healthy melatonin cycles for better nighttime sleep.
- Limit evening screens. Blue light delays melatonin release. Wear blue-blocking glasses if evening exposure is unavoidable.
- Follow the Anti-Inflammatory Rainbow Diet™. Eat colorful fruits and vegetables like berries, spinach, and nuts. These enhance how sleep affects health by:
- Fighting oxidative stress with antioxidants, easing pain in fibromyalgia, arthritis, and chronic fatigue.
- Improving gut health with fiber and probiotics, increasing serotonin for mood and sleep in all ages.
- For a delicious option that supports restful sleep, check out my recipe for the Salmon Quinoa Bowl with Tart Cherries.
- Eat your last meal 3 hours before bed. Avoid late sugar spikes and crashes that disrupt sleep.
- Practice mindfulness. Try 5–10 minutes of deep breathing or meditation before bed. This lowers stress hormones, improving focus in kids and easing chronic pain.
- Exercise regularly. Aim for morning or afternoon walks or yoga. This deepens sleep and reduces inflammation. However, avoid vigorous exercise within 3 hours of bedtime.
- Use melatonin wisely. Consider a low dose short-term, ideally after addressing underlying issues like stress or diet, ideally under professional guidance.
- Be cautious with sleep medications: Avoid long-term use of benzodiazepines and antihistamines that impair brain restorative processes.
- Listen to your body: Poor sleep may manifest as unusual symptoms, like feeling cold despite heat or chronic pain flare-ups—these are signals to take sleep seriously.
Consequently, these steps enhance energy, reduce pain, and sharpen thinking for all.
The Takeaway
Good sleep is not a luxury. It’s essential. Every night, it acts as a reset button for your brain, gut, and body, helping keep you healthy and balanced. Whether you want to protect your brain from dementia, manage IBS or weight, keep fibromyalgia flares at bay, or simply feel your best each morning, prioritizing good sleep may be the single most powerful health choice you can make.
If you’ve struggled with sleep, please share your experiences in the comments—what has worked and what hasn’t. Your insights might help others on the same journey.
For a deeper dive into how to protect your health through better sleep and how the Anti-Inflammatory Rainbow Diet™ can help, explore my book God’s Prescription. You’ll also find more tips on raising healthy kids in Chapter 13.
Sources
Cognition
- Martins C.R. The impact of sleep deprivation on cognitive performance in young adults. Int J Psychol Sci. 2021;3(1):22-25. doi:10.33545/26648377.2021.v3.i1a.70. https://www.psychologyjournal.net/archives/2021/vol3issue1/PartA/7-1-16-453.pdf
- Sun X, Qu Z, Zhang X, Zhang Y, Zhang X, Zhao H, Zhang H. The effects of sleep deprivation on cognitive flexibility: a scoping review of outcomes and biological mechanisms. Front Neurosci. 2025 Jul 22;19:1626309. doi: 10.3389/fnins.2025.1626309. PMID: 40766906; PMCID: PMC12321868. https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1626309/full
Glymphatic System
- Ma J, Chen M, Liu G.H., Gao M, Chen N.H., Toh C.H., Hsu J.L., Wu K.Y., Huang C.M., Lin C.M., Fang J.T., Lee S.H., Lee T.M.C. Effects of sleep on the glymphatic functioning and multimodal human brain network affecting memory in older adults. Mol Psychiatry. 2025 May;30(5):1717-1729. doi: 10.1038/s41380-024-02778-0. Epub 2024 Oct 14. PMID: 39397082; PMCID: PMC12014484. https://www.nature.com/articles/s41380-024-02778-0
Stroke and Dementia Risk
- Clocchiatti-Tuozzo S., Rivier C.A., Renedo D., Torres Lopez V.M., Geer J.H., Miner B., Yaggi H.K., de Havenon A., Payabvash S., Sheth K.N., Gill T.M., Falcone G.J. Suboptimal Sleep Duration Is Associated With Poorer Neuroimaging Brain Health Profiles in Middle-Aged Individuals Without Stroke or Dementia. J Am Heart Assoc. 2024 Jan 2;13(1):e031514. doi: 10.1161/JAHA.123.031514. Epub 2023 Dec 29. PMID: 38156552; PMCID: PMC10863828. https://www.ahajournals.org/doi/10.1161/JAHA.123.031514?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
- Sabia S., Fayosse A., Dumurgier J. et al. Association of sleep duration in middle and old age with incidence of dementia. Nat Commun 12, 2289 (2021). https://doi.org/10.1038/s41467-021-22354-2.https://www.nature.com/articles/s41467-021-22354-2#citeas
- Yiallourou S, Baril A.A., Wiedner C., Misialek J.R., Kline C.E., Harrison S., Cannon E., Yang Q., Bernal R., Bisson A., Himali D., Cavuoto M., Weihs A., Beiser A., Gottesman R.F., Leng Y., Lopez O., Lutsey P.L., Purcell S.M., Redline S., Seshadri S., Stone K.L., Yaffe K., Ancoli-Israel S., Xiao Q., Vaou E.O., Himali J.J., Pase M.P. Sleep architecture and dementia risk in adults: An analysis of 5 cohorts from the Sleep and Dementia Consortium. Sleep. 2025 May 16:zsaf129. doi: 10.1093/sleep/zsaf129. Epub ahead of print. PMID: 40377976. https://pubmed.ncbi.nlm.nih.gov/40377976/
Sleep Aids
- Ettcheto M., Olloquequi J., Sánchez-López E., Busquets O., Cano A., Manzine P.R., Beas-Zarate C., Castro-Torres R.D., García M.L., Bulló M., Auladell C., Folch J., Camins A. Benzodiazepines and Related Drugs as a Risk Factor in Alzheimer’s Disease Dementia. Front Aging Neurosci. 2020 Jan 8;11:344. doi: 10.3389/fnagi.2019.00344. PMID: 31969812; PMCID: PMC6960222. https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2019.00344/full
- Gray S.L., Anderson M.L., Dublin S., Hanlon J.T., Hubbard R., Walker R., Yu O., Crane P.K., Larson E.B. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. 2015 Mar;175(3):401-7. doi: 10.1001/jamainternmed.2014.7663. PMID: 25621434; PMCID: PMC4358759. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2091745
Thermoregulation
- Landis C.A., Savage M.V., Lentz M.J., Brengelmann G.L. Sleep Deprivation Alters Body Temperature Dynamics to Mild Cooling and Heating Not Sweating Threshold in Women, Sleep, Volume 21, Issue 1, January 1998, Pages 101–108, https://doi.org/10.1093/sleep/21.1.101
- Romeijn N., Verweij I.M., Koeleman A., Mooij A. Steimke R., Virkkala J., van der Werf Y., Van Someren E.J.W. Cold Hands, Warm Feet: Sleep Deprivation Disrupts Thermoregulation and Its Association with Vigilance, Sleep, Volume 35, Issue 12, 1 December 2012, Pages 1673–1683, https://doi.org/10.5665/sleep.2242
Autonomic Nervous System
- Messa R.M., Benfica M.A., Ribeiro L.F.P., Williams C.M., Davidson S.R.E., Alves E.S. The effect of total sleep deprivation on autonomic nervous system and cortisol responses to acute stressors in healthy individuals: A systematic review. 2024 Oct;168:107114. doi: 10.1016/j.psyneuen.2024.107114. Epub 2024 Jun 28. PMID: 38991306. https://www.sciencedirect.com/science/article/pii/S0306453024001586
Dysbiosis and Intestinal Permeability
- Sun J., Fang D., Wang Z., Liu Y. Sleep Deprivation and Gut Microbiota Dysbiosis: Current Understandings and Implications. Int J Mol Sci. 2023 May 31;24(11):9603. doi: 10.3390/ijms24119603. PMID: 37298553; PMCID: PMC10253795. https://www.mdpi.com/1422-0067/24/11/9603
Oxidative Stress
- Davinelli S., Medoro A., Savino R., Scapagnini G. Sleep and Oxidative Stress: Current Perspectives on the Role of NRF2. Cell Mol Neurobiol. 2024 Jun 25;44(1):52. doi: 10.1007/s10571-024-01487-0. PMID: 38916679; PMCID: PMC11199221. https://link.springer.com/article/10.1007/s10571-024-01487-0
Hormones & Obesity
- Chaput J.P., McHill A.W., Cox R.C., Broussard J.L., Dutil C., da Costa B.G.G., Sampasa-Kanyinga H., Wright K.P. Jr. The role of insufficient sleep and circadian misalignment in obesity. Nat Rev Endocrinol. 2023 Feb;19(2):82-97. doi: 10.1038/s41574-022-00747-7. Epub 2022 Oct 24. PMID: 36280789; PMCID: PMC9590398. https://pmc.ncbi.nlm.nih.gov/articles/PMC9590398/
- Davidson J.R., Moldofsky H., Lue F.A. Growth hormone and cortisol secretion in relation to sleep and wakefulness. J Psychiatry Neurosci. 1991 Jul;16(2):96-102. PMID: 1911740; PMCID: PMC1188300. https://pmc.ncbi.nlm.nih.gov/articles/PMC1188300/
- van Egmond L.T., Meth E.M.S., Engström J., Ilemosoglou M., Keller J.A., Vogel H., Benedict C. Effects of acute sleep loss on leptin, ghrelin, and adiponectin in adults with healthy weight and obesity: A laboratory study. Obesity (Silver Spring). 2023 Mar;31(3):635-641. doi: 10.1002/oby.23616. Epub 2022 Nov 20. PMID: 36404495. https://onlinelibrary.wiley.com/doi/10.1002/oby.23616
Immune Function & Cytokines
- Besedovsky L., Lange T., Born J.. Sleep and immune function. Pflugers Arch. 2012 Jan;463(1):121-37. doi: 10.1007/s00424-011-1044-0. Epub 2011 Nov 10. PMID: 22071480; PMCID: PMC3256323. https://pmc.ncbi.nlm.nih.gov/articles/PMC3256323/
- Garbarino S., Lanteri P., Bragazzi N.L., Magnavita N., Scoditti E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol. 2021 Nov 18;4(1):1304. doi: 10.1038/s42003-021-02825-4. PMID: 34795404; PMCID: PMC8602722. https://www.nature.com/articles/s42003-021-02825-4
Children
- Chaput J.P., Dutil C. Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. Int J Behav Nutr Phys Act. 2016 Sep 26;13(1):103. doi: 10.1186/s12966-016-0428-0. PMID: 27669980; PMCID: PMC5037605. https://ijbnpa.biomedcentral.com/articles/10.1186/s12966-016-0428-0
- Chen H.., Wang LJ., Xin F., Liang G., Chen Y. Associations between sleep duration, sleep quality, and weight status in Chinese children and adolescents. BMC Public Health. 2022 Jun 7;22(1):1136. doi: 10.1186/s12889-022-13534-w. PMID: 35668374; PMCID: PMC9172025. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-13534-w
- Farraj R.H., Haddad S., Cohen C., and Mualem R., (2025), Impact of Sleep Duration on Cognitive Performance and Emotional State Changes in High School Students, Neuroscience and Neurological Surgery, 17(1); DOI:10.31579/2578-8868/348. https://auctoresonline.org/article/impact-of-sleep-duration-on-cognitive-performance-and-emotional-state-changes-in-high-school-students
- Jiang X., Hardy L.L., Baur L.A., Ding D., Wang L., Shi H. Sleep duration, schedule and quality among urban Chinese children and adolescents: associations with routine after-school activities. PLoS One. 2015 Jan 22;10(1):e0115326. doi: 10.1371/journal.pone.0115326. PMID: 25611973; PMCID: PMC4303432. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0115326
- Johri K., Pillai R., Kulkarni A. et al. Effects of sleep deprivation on the mental health of adolescents: a systematic review. Sleep Science Practice 9, 9 (2025). https://doi.org/10.1186/s41606-025-00127-w.https://sleep.biomedcentral.com/articles/10.1186/s41606-025-00127-w#citeas
- LeBourgeois M.K., Hale L., Chang A.M., Akacem L.D., Montgomery-Downs H.E., Buxton O.M. Digital Media and Sleep in Childhood and Adolescence. Pediatrics. 2017 Nov;140(Suppl 2):S92-S96. doi: 10.1542/peds.2016-1758J. PMID: 29093040; PMCID: PMC5658795. https://publications.aap.org/pediatrics/article/140/Supplement_2/S92/34177/Digital-Media-and-Sleep-in-Childhood-and?autologincheck=redirected
- Liu J., Ji X., Pitt S., Wang G., Rovit E., Lipman T., Jiang F. Childhood sleep: physical, cognitive, and behavioral consequences and implications. World J Pediatr. 2024 Feb;20(2):122-132. doi: 10.1007/s12519-022-00647-w. Epub 2022 Nov 23. PMID: 36418660; PMCID: PMC9685105. https://pmc.ncbi.nlm.nih.gov/articles/PMC9685105/
- Owens J., Adolescent Sleep Working Group; Committee on Adolescence. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014 Sep;134(3):e921-32. doi: 10.1542/peds.2014-1696. PMID: 25157012; PMCID: PMC8194472. https://publications.aap.org/pediatrics/article/134/3/e921/74176/Insufficient-Sleep-in-Adolescents-and-Young-Adults
- Wang W., Zhu Y., Yu H., Wu C., Li T., Ji C., Jiang Y., Ding D. The impact of sleep quality on emotion regulation difficulties in adolescents: a chained mediation model involving daytime dysfunction, social exclusion, and self-control. BMC Public Health. 2024 Jul 11;24(1):1862. doi: 10.1186/s12889-024-19400-1. PMID: 38992632; PMCID: PMC11241850. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-19400-1
- Wheaton A.G., Claussen A.H. Short Sleep Duration Among Infants, Children, and Adolescents Aged 4 Months-17 Years – United States, 2016-2018. MMWR Morb Mortal Wkly Rep. 2021 Sep 24;70(38):1315-1321. doi: 10.15585/mmwr.mm7038a1. PMID: 34555000; PMCID: PMC8459893. https://www.cdc.gov/mmwr/volumes/70/wr/mm7038a1.htm?s_cid=mm7038a1_
- Zaffanello M., Pietrobelli A., Cavarzere P., Guzzo A., Antoniazzi F. Complex relationship between growth hormone and sleep in children: insights, discrepancies, and implications. Front Endocrinol (Lausanne). 2024 Jan 24;14:1332114. doi: 10.3389/fendo.2023.1332114. PMID: 38327902; PMCID: PMC10847528. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1332114/full
Screentime
- Hjetland G.J., Skogen J.C., Hysing M., Gradisar M., Sivertsen B. How and when screens are used: comparing different screen activities and sleep in Norwegian university students. Front Psychiatry. 2025 Mar 31;16:1548273. doi: 10.3389/fpsyt.2025.1548273. PMID: 40270574; PMCID: PMC12015757. https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1548273/full