You’ve probably heard about weight-loss medications like Ozempic and Wegovy, especially in conversations about GLP-1 and weight loss. They’re everywhere—celebrity endorsements, news headlines, even casual conversation at the gym. But here’s what most people don’t know: GLP-1 isn’t a pharmaceutical invention. It’s a natural hormone made by your body.
GLP-1 stands for glucagon-like peptide-1. After you eat, your intestines produce this hormone. When your digestive system is working well, GLP-1 performs three critical jobs:
1. It signals your brain that you’re satisfied.
It tells your hypothalamus—the control center for hunger and fullness—that you’ve had enough. So, it’s not about willpower. It’s about gut-brain communication.
2. It slows digestion to prevent blood sugar spikes.
By regulating how quickly food leaves your stomach, GLP-1 helps keep your blood sugar steady. No dramatic peaks. No energy crashes an hour later.
3. It helps your pancreas release the right amount of insulin.
GLP-1 fine-tunes insulin secretion based on what you’ve eaten. This is why it’s called an “incretin” hormone—it increases insulin response, but only when blood sugar is elevated.
In a healthy system, this all happens automatically. You eat. Your gut releases GLP-1. Your blood sugar stays balanced. You feel satisfied, not stuffed. Your energy stays even.
So, the question isn’t whether GLP-1 works. It’s why your body might have stopped responding to its signal.
What Most People Don’t Know About GLP-1
GLP-1 isn’t just about weight loss and appetite suppression.It affects:
- Insulin sensitivity – how well your cells respond to insulin and use glucose for energy
- Digestion speed – how long nutrients stay in your stomach and small intestine
- Inflammation – GLP-1 can help calm chronic inflammation in many parts of the body
- Fat storage patterns – including visceral fat around your organs
Sadly, factors common in the world we live in can weaken your body’s natural GLP-1 response. Signal weakening can happen when:
-
- Chronic stress keeps cortisol elevated
- Ultra-processed foods disrupt gut signaling
- Poor sleep interferes with hormone regulation
- Food sensitivities trigger inflammation
- Gut dysfunction (leaky gut, dysbiosis aka microbial imbalance, inflammation) impairs GLP-1 production
When GLP-1 signaling weakens, gut-brain communication and blood sugar control both break down. You get hungrier faster. You crave more—especially sugar and refined carbs. You feel less satisfied after meals. And your body stores fat more easily, particularly around your midsection.
This is metabolic disruption, not moral failure.
What this looks like in real life:
You eat a balanced breakfast—eggs, vegetables, maybe some fruit—and you’re hungry again within two hours. Or you finish a full meal and find yourself standing in front of the pantry an hour later, looking for something sweet even though you’re not physically hungry.
You might notice you can’t seem to lose weight around your midsection no matter how “good” you eat. Or your energy crashes hard in the afternoon, and the only thing that helps is more food—usually something quick and carb-heavy.
These aren’t character flaws or lack of discipline. They’re signs that your body’s satiety signaling has been disrupted. When GLP-1 production is low or your cells have become resistant to its signal, your brain literally doesn’t receive clear messages about fullness, blood sugar stability, or energy availability.
As a result, you feel like you’re constantly fighting your own body because you are. Your communication system has been compromised.
The Microbiome Connection Nobody’s Talking About
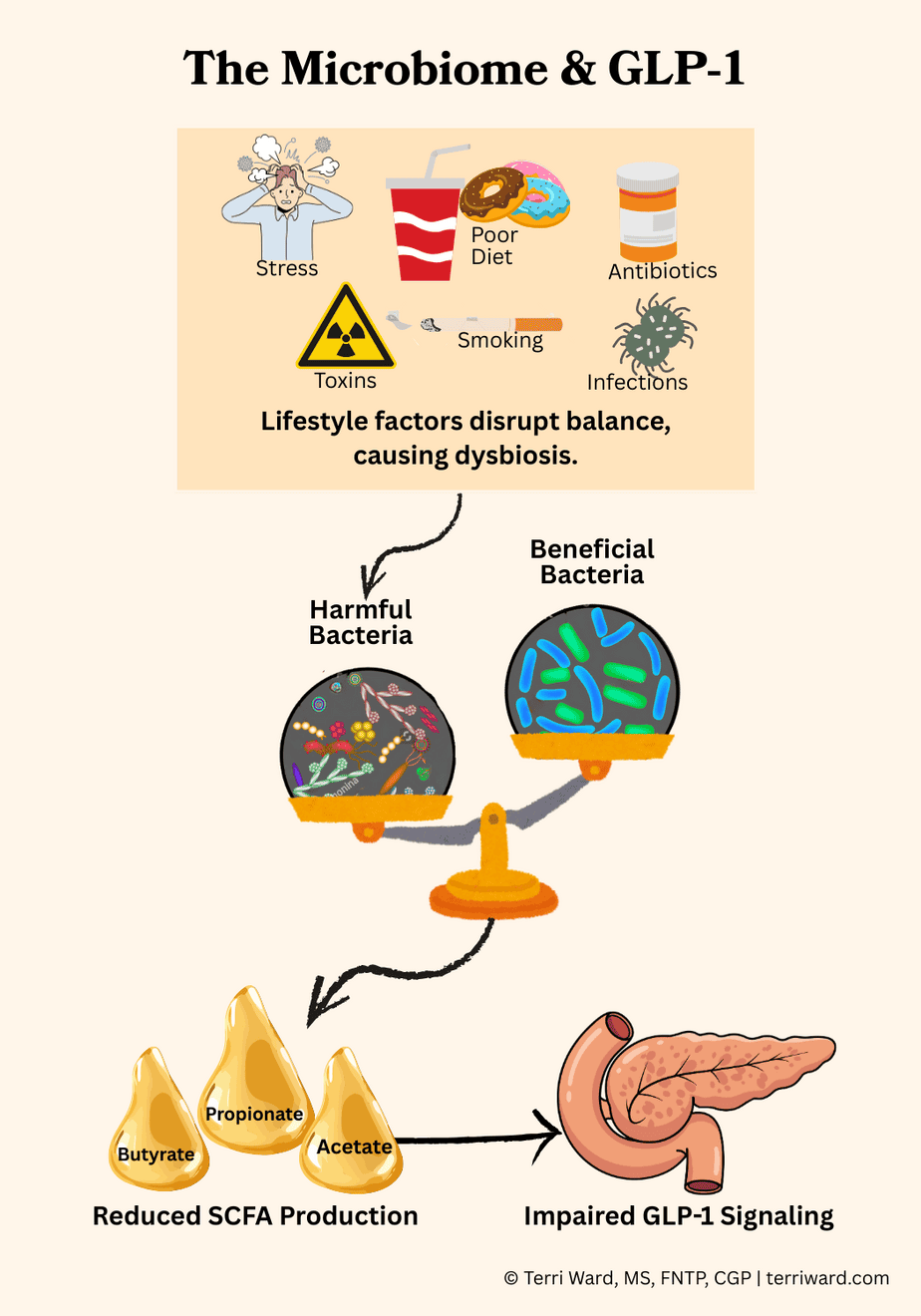
Your gut bacteria directly influence how much GLP-1 your body produces. Specialized L-cells in your intestinal lining release GLP-1. These cells don’t work alone—they respond to signals from your microbiome, the trillions of bacteria living in your gut.
When you eat fiber, certain beneficial bacteria ferment it into short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate. These SCFAs signal your L-cells to release GLP-1. They also fuel the cells lining your gut to maintain barrier integrity, reduce inflammation throughout your body, and help regulate your immune system.
A healthy, diverse microbiome amplifies GLP-1 production. A disrupted one can significantly blunt it.
Your gut microbiome can be damaged by:
-
- Antibiotics (even ones you took years ago)
- Chronic stress
- A diet low in fiber and high in processed foods
- Environmental toxins
- Smoking
- Gut infections or overgrowths
When your beneficial bacteria decline, SCFA production drops. Your L-cells get quieter. Even with a healthy diet, if your microbiome is disrupted, your body may not produce adequate GLP-1. The signaling breaks down before it even starts.
This explains why two people can eat the same meal and have completely different satiety responses. Ultimately, it’s not just about the food. It’s about whether your gut bacteria can turn that food into the signals your body needs.
GLP-1 Weight Loss Drugs vs. Supporting Natural GLP-1 and Weight Loss
GLP-1 medications are designed to mimic this hormone by giving the body a stronger, longer‑lasting GLP‑1‑like signal than it would normally make on its own. They override the broken signaling system. For some people, particularly those with severe insulin resistance or type 2 diabetes, these medications can be life-changing, but they need to be taken long-term and come with side effects.
The pharmaceutical industry would probably prefer you didn’t know that your body is designed to make its own GLP-1 when digestion is healthy and your microbiome is intact. Unfortunately, many people’s systems have become so disrupted that they may not produce or respond to natural GLP‑1 effectively anymore.
GLP-1 medications can be powerful tools, but they don’t repair the reasons GLP‑1 signaling became disrupted in the first place. Fortunately, there are evidence-based ways to support your body’s natural GLP-1 production.
How to Support Natural GLP-1 Production
- Feeding your microbiome fiber
Your beneficial gut bacteria need fiber to produce the short-chain fatty acids that signal GLP-1 release. Focus on diverse fiber sources: vegetables, fruits, legumes, nuts, and seeds. Variety matters—different types of fiber feed different bacterial strains. Aim for 25 to 35 grams daily from whole food sources, not supplements.
- Stabilizing blood sugar with protein-first meals
Starting your meals with protein slows glucose absorption and triggers GLP-1 release naturally. Protein also increases satiety independently of GLP-1, giving you double benefit. Aim for 25 to 30 grams of quality protein at each meal from eggs, fish, poultry, grass-fed meat, or legumes.
- Managing chronic stress
Elevated cortisol suppresses digestive function and disrupts the gut environment where GLP-1 is produced. Chronic stress also drives insulin resistance, which impairs GLP-1 signaling. Stress management isn’t optional—it’s foundational to metabolic health. This includes sleep quality, nervous system regulation, and addressing the emotional and spiritual roots of chronic stress.
- Healing gut barrier integrity
A damaged gut lining (leaky gut) allows inflammatory compounds into your bloodstream, triggering systemic inflammation that disrupts hormone signaling throughout your body, including GLP-1. Healing requires removing inflammatory triggers (processed foods, excess sugar, food sensitivities), supporting the gut lining with nutrient-dense foods, and restoring beneficial bacteria.
Your body isn’t broken. The signaling might be disrupted, but it can be restored.
I praise you because I am fearfully and wonderfully made. (Psalm 139:14 NIV)
Probiotics for GLP-1 and Weight Loss
While food should always be your foundation, certain probiotic strains may offer additional support for GLP-1 production and weight management by protecting the intestinal cells that produce GLP-1 and enhancing SCFA production.
Strains with GLP-1 research
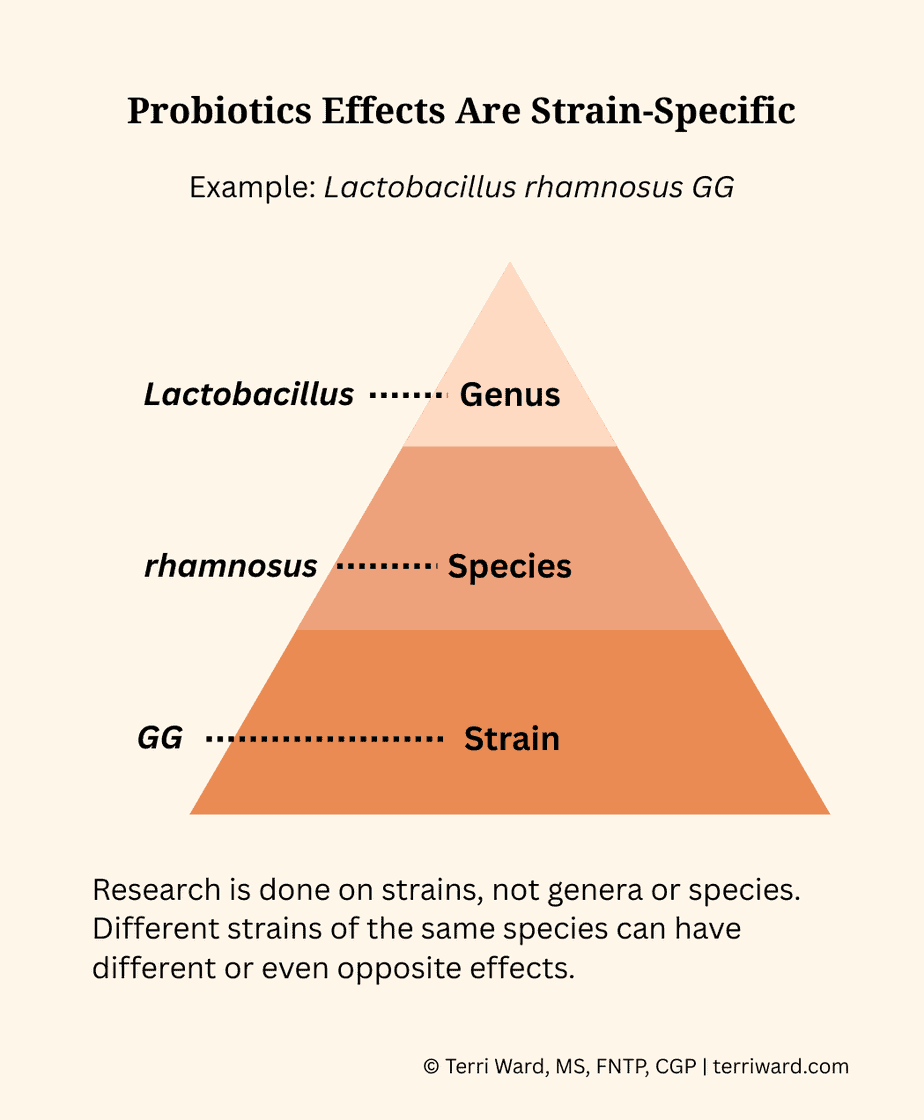
Probiotic effects are strain-specific, not species-specific. You cannot assume research on one strain applies to another, even within the same species, and unfortunately many labels do not disclose strains. The following strains may support GLP-1 production:
-
- Lactobacillus rhamnosus GG has been studied for its ability to protect the intestinal cells that produce GLP-1 from damage and support SCFA production.
- VSL#3 is a multi-strain formulation. The company does not disclose those strains, but evidence supports the formulation supporting GLP-1 and metabolic health.
Strains with weight loss research
Research has shown that several single-strain probiotics produce positive effects in decreasing body weight, BMI, waist circumference, body fat mass, or fat percentage. These include:
-
- Lactobacillus strains: L. rhamnosus CGMCC1.3724, L. gasseri BNR17, L. gasseri SBT2055, L. sakei CJLS03, and L. plantarum Dad-13
- Bifidobacterium strains: B. lactis Bb-12, B. animalis ssp. lactis 420, and B. animalis CECT8145
- Pediococcus pentosaceus LP28
Be sure you know the specific strain designation on any probiotic you’re considering. The species name alone isn’t enough, and the effects of a different strain may be the opposite of what you’re want to achieve.
If you’re ready to explore targeted supplementation as part of a comprehensive health strategy, click here to schedule a free 30-minute strategy session to discuss your health goals and determine your best next steps.
The Bigger Picture
Understanding GLP-1 is one piece of a larger puzzle. This post explains how stress drives belly fat storage, making weight loss feel impossible, and in coming posts, I’ll connect the dots between hormones, metabolism, gut health, and nutrition, including:
-
- Why you can’t fix weight or stress without fixing your gut first
- Protein first: the simplest way to stabilize blood sugar and protect muscle
- Why fiber might be the most underrated tool for metabolic health
- The Anti-Inflammatory Rainbow Diet framework—a practical, sustainable way to eat that works with your body’s design, not against it
Want weekly Scripture, wellness tips, and anti-inflammatory recipes?
Subscribe to Wednesday’s Wisdom and Wellness below.
No spam. Unsubscribe anytime.
Ready to understand what’s happening in your body? Schedule a free 30-minute strategy session with Terri to discuss your health concerns and determine your best next steps.


GLP-1 medications seem promising for weight loss, but I worry about potential side effects and long-term dependency. More research is definitely needed.
I agree. They are life-changing for some, particularly those who can’t seem to change their diet or lifestyle, but they’re not without risks. I believe we shouldn’t lose weight to get healthy, but rather get healthy to lose weight.