You’re eating clean, exercising regularly, maybe even fasting—but the weight around your middle won’t budge. What if the problem isn’t what you’re eating or how much you’re moving? What if it’s stress-related cortisol belly fat—and your body is deciding where your body stores fat?
Cortisol is your primary stress hormone, produced by your adrenal glands in response to physical or psychological stress. It’s not inherently bad—in fact, you need it to survive. Cortisol helps you:
-
- Wake up in the morning and feel alert
- Mobilize energy when you need it
- Regulate blood sugar between meals
- Manage inflammation
- Respond to threats or challenges
The problem isn’t cortisol itself. It’s when cortisol stays chronically elevated or when your natural cortisol rhythm gets disrupted.
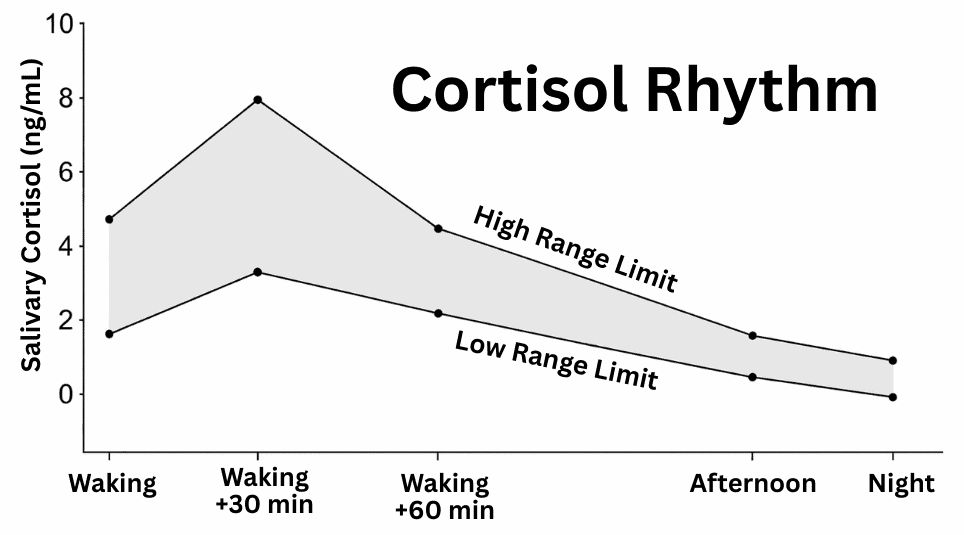
Understanding Your Cortisol Rhythm
Cortisol naturally rises in the morning to help you wake up and mobilize energy. Its normal pattern is as follows:
Morning (6-9 AM): Cortisol peaks to help you wake up, mobilize energy, and prepare for the day. This is called the cortisol awakening response (CAR).
Mid-morning to afternoon: Cortisol gradually declines as you move through your day.
Evening: Cortisol should be at its lowest, allowing melatonin to rise so you can sleep.
Overnight: Cortisol stays low, then begins rising again a few hours before you wake.
This rhythm is healthy and necessary. The problems start when:
-
- Cortisol stays elevated all day (chronic stress)
- The morning peak is blunted (you can’t wake up)
- Cortisol spikes at night (you can’t fall asleep or you wake at 2 to 4 AM)
- The rhythm becomes completely flattened or erratic
Understanding Cortisol Belly Fat
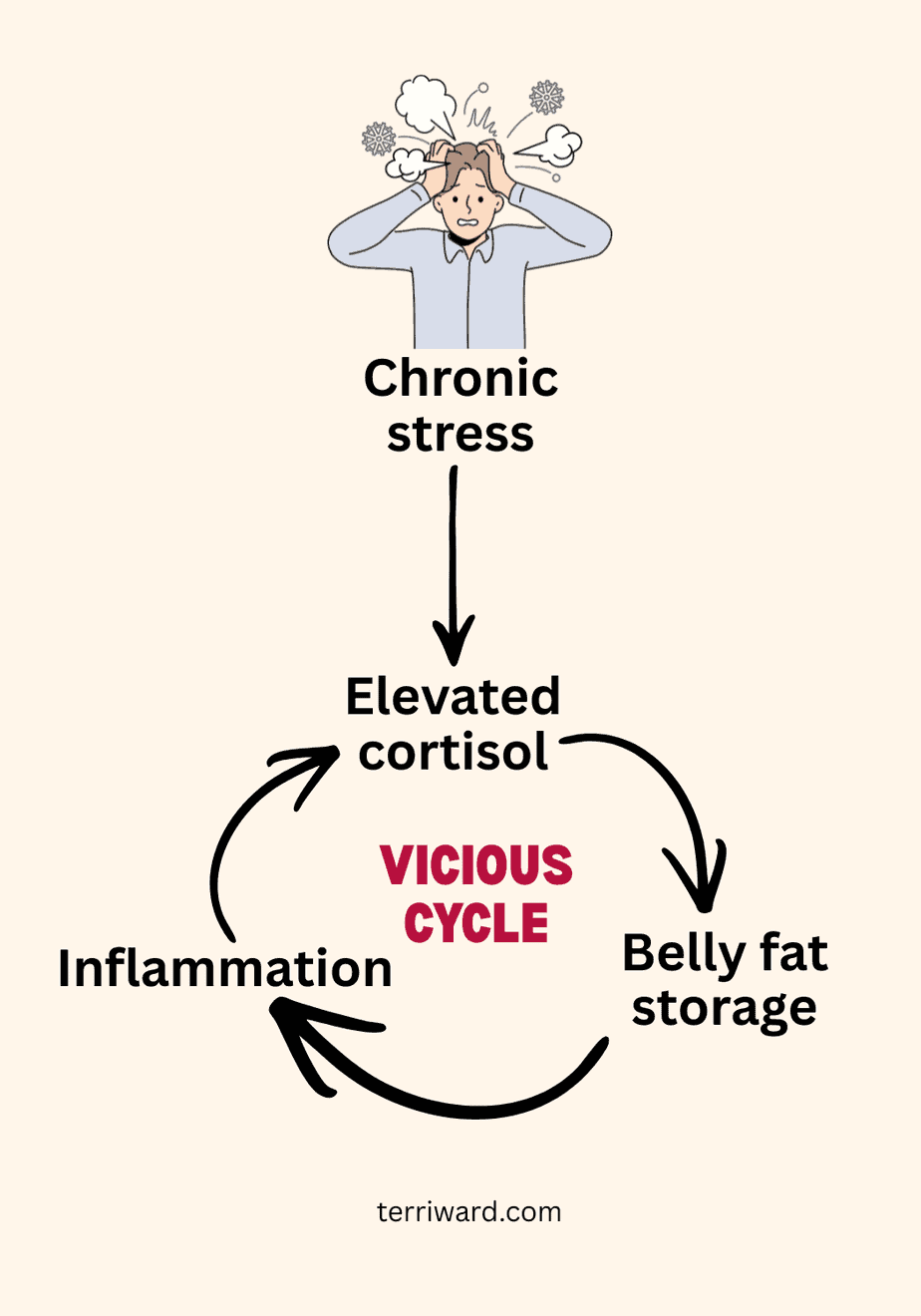
When cortisol stays chronically elevated, it doesn’t just make you store more fat—it changes where your body stores it.
Cortisol drives preferential abdominal fat storage, particularly visceral fat—the fat that wraps around your organs. This isn’t random. Visceral fat tissue has more cortisol receptors than subcutaneous fat (the fat you can pinch under your skin). When cortisol levels rise, these receptors signal fat cells in your abdomen to store more energy.
Visceral fat is more dangerous than subcutaneous fat because it is metabolically active. It produces inflammatory cytokines that travel throughout your body, triggering more inflammation and more cortisol production, creating a vicious cycle.
This is why cortisol belly fat is so stubborn. You’re not just dealing with excess calories. You’re dealing with a disrupted hormonal feedback loop.
Cortisol Isn’t the Only Cause of Belly Fat
It’s important to acknowledge that cortisol isn’t the only reason people gain belly fat. Hormonal changes during menopause and perimenopause, environmental toxicity (like heavy metals), insulin resistance, thyroid dysfunction, and certain medications can all contribute to abdominal weight gain. In my own case, unexplained weight gain was one of the final clues that led me to uncover underlying uranium toxicity from our well water.
But if you’ve noticed your belly fat is tied to stressful periods in your life, or if the self-assessment below resonates with you, cortisol and stress may be worth addressing.
Is Stress Driving Your Weight Gain?
Check the signs that suggest chronic stress is affecting your metabolism:
□ Weight gain concentrated around your midsection, even when other areas stay the same
□ Energy crashes in the afternoon, followed by cravings for sugar or caffeine
□ Difficulty falling asleep despite feeling exhausted
□ Waking between 2 and 4 AM with racing thoughts
□ Feeling “wired and tired” at the same time
□ Irritability or mood swings, especially when hungry
□ Increased belly fat despite eating well and exercising
□ Difficulty recovering from workouts
□ Brain fog or trouble concentrating
□ Increased anxiety or feeling constantly on edge
If you checked 3 or more, your stress hormones may be working against your health goals.
HPA Axis Dysregulation (formerly known as Adrenal Fatigue)
You may have heard the term “adrenal fatigue, ” and you may have also heard it’s controversial or “not real.” Here’s what’s actually happening:
Your adrenal glands don’t get “fatigued” in the way the term suggests. However, the HPA axis (hypothalamic-pituitary-adrenal axis)—the communication network between your brain and adrenal glands—absolutely can become dysregulated.
The term “adrenal fatigue” isn’t a formal medical diagnosis and doesn’t have its own ICD code, so many conventional doctors don’t acknowledge it. Functional and integrative medicine practitioners instead talk about HPA-axis dysfunction—a real, measurable pattern of disrupted cortisol production and stress-response signaling.
The result? Your cortisol rhythm gets flattened, reversed, or erratic. You might have high cortisol when it should be low (can’t sleep at night) and low cortisol when it should be high (can’t wake up in the morning).
This isn’t just “being tired.” It’s a physiological pattern with measurable consequences.
Years ago, I went from elevated cortisol to low cortisol (what was called stage 4 adrenal exhaustion back then). When someone recently asked me how I restored my HPA axis, I realized I couldn’t point to one thing, and to be honest, I still have to work on it. For me, recovery was a gradual process involving career change, nervous system work, faith practices, nutrient support, and time.
Looking back, I can see that my body needed me to stop doing and start being—something my perfectionist, Type A personality resisted. But God’s design isn’t constant worry or stress, and my body couldn’t heal until I learned that lesson.
Come to me, all you who are weary and burdened, and I will give you rest.
(Matthew 11:28 NIV)
Rest is not only a spiritual invitation; it is also a biological necessity. Chronic stress and worry show up physically through cortisol’s effects on the body—not only in increased belly fat, but also in how it influences blood sugar.
The Blood Sugar-Cortisol Connection
Cortisol and blood sugar are intimately connected. One of cortisol’s primary jobs is to maintain blood sugar between meals by mobilizing stored glucose from your liver and muscles.
When blood sugar drops—whether from skipping meals, fasting, or eating a carb-heavy meal that causes a crash—cortisol rises to bring it back up. This is normal and healthy in the short term.
The problem arises for people with:
-
- Dysregulated blood sugar (insulin resistance, prediabetes)
- High baseline stress (chronic work stress, relationship stress, financial stress)
- HPA axis dysfunction (disrupted cortisol rhythm)
With these conditions, extending fasting windows much beyond a gentle overnight fast (around 12 hours) can prolong cortisol elevation. Instead of the cortisol awakening response tapering off naturally as you eat and start your day, it may remain higher for longer. This extended cortisol elevation may:
-
- Disrupt insulin signaling (making it harder for your cells to use glucose)
- Increase cravings later in the day (especially for sugar and refined carbs)
- Increase protein breakdown to make glucose, which over time may reduce lean mass if recovery and intake are inadequate
- Signal your body to store fat, particularly in the abdominal area
With higher baseline stress or sensitive blood sugar regulation, delaying food—especially protein—can work against their goals. For many, eating a protein-forward breakfast early in the day (ideally before 10 AM) can help calm the stress response, stabilize blood sugar, and support fat loss without sacrificing muscle.
One of my favorite cortisol-smart breakfasts is this Anti-Inflammatory Shakshuka – packed with protein, vegetables, and stress-reducing spices that work together to support your body’s natural rhythm.
Scripture acknowledges the wisdom of eating at proper times.
Happy is the land whose king is a noble leader and whose leaders feast at the proper time to gain strength for their work, not to get drunk.
(Ecclesiastes 10:17 NLT)
Why Fasting Isn’t Universal (And That’s Okay)
Intermittent fasting has become incredibly popular, and for good reason—it works beautifully for many people. When your metabolism is healthy and your stress response is regulated, giving your body longer breaks between meals or extended periods without food can often improve insulin sensitivity, support cellular repair, and even aid fat loss.
A gentle overnight fast of around 12 hours is generally well tolerated for most people, including those with some metabolic issues. The challenges tend to arise with more aggressive fasting protocols—very long daily fasting windows, routinely skipping breakfast in a high‑stress life, or alternate‑day fasting.
But fasting isn’t universal. For some people—especially those with HPA axis dysregulation, blood sugar issues, or chronic stress—these more aggressive fasting approaches can act like another stressor and backfire. When your body reads fasting as “danger,” cortisol may stay elevated, blood sugar can swing more wildly, and your system may respond by conserving energy and holding onto fat—particularly around your middle.
Signs fasting may not be working for you:
-
- Increased belly fat despite following your fasting plan
- Afternoon energy crashes and intense cravings
- Feeling anxious, irritable, or “hangry” during fasting windows
- Waking up at night or having trouble falling asleep
- Feeling cold, especially in your hands and feet
- Difficulty recovering from workouts
- Loss of menstrual cycle regularity (for women)
If you’re experiencing these symptoms, your body may be interpreting fasting as another stressor rather than a healing tool.
This doesn’t mean you’ve failed at fasting. It means your body needs a different approach right now. One thing people with disrupted HPA axis function or sensitive blood sugar regulation can do is eat protein earlier in the day (ideally before 10 AM). This signals safety to your nervous system, stabilizes blood sugar, and allows cortisol to taper naturally instead of staying elevated for hours.
Cortisol and GLP-1
Cortisol also disrupts the metabolic signaling I wrote about in my post on GLP‑1 and weight loss. When cortisol stays chronically elevated, it can impair insulin signaling, disrupt hormones that regulate hunger and fullness, and tell your body to store more fat—especially around your organs. You can read the post HERE.
The Bigger Picture
Cortisol and GLP-1 are pieces of a larger puzzle. In the coming posts, I’ll connect the dots between weight loss, gut health, and nutrition, including:
-
- Why you can’t fix weight or stress without fixing your gut first
- Protein first: the simplest way to stabilize blood sugar and protect muscle
- Why fiber might be the most underrated tool for metabolic health
- The Anti-Inflammatory Rainbow Diet framework—a practical, sustainable way to eat that works with your body’s design, not against it
If you’re struggling with stubborn belly fat despite eating well and exercising, elevated cortisol may be the missing piece of your puzzle. Schedule a free 30-minute strategy session to discuss your symptoms and explore whether cortisol management could be your path forward.
Want weekly Scripture, wellness tips, and anti-inflammatory recipes?
Subscribe to Wednesday’s Wisdom and Wellness below.
No spam. Unsubscribe anytime.