GLP-1 medications promise weight loss and better blood sugar control by mimicking signals your body already knows how to produce. What most people don’t realize is that the relationship between fiber and blood sugar regulation is one of those built-in signals. Your body was designed to release GLP-1 naturally, and fiber is one of the primary triggers that turns it on.
Yet most Americans consume far less than the recommended 25+ grams of fiber per day. It’s not because they don’t care, but because our modern food system makes it surprisingly difficult to eat enough whole, fiber-rich foods consistently.
During my Master of Science program in Human Nutrition and Functional Medicine, I learned how closely fiber and blood sugar are connected. I also learned that fiber doesn’t just affect digestion. It influences appetite signaling, insulin sensitivity, hormone balance, gut microbiome health, and metabolic communication between organs. That’s likely why fiber has suddenly re-entered the wellness spotlight. But functional nutrition has understood this relationship for decades.
Taking Fiber from Theory to Real Life
But it wasn’t until I wrote The Healing Diverticulitis Cookbook that I truly understood the practical challenge of incorporating adequate fiber into our diet.
As I developed recipes and mapped out daily meal plans, it became obvious that hitting fiber targets doesn’t happen accidentally. It requires intentional food choices and preparation methods, meal planning, and creating household systems that make fiber-rich eating the default, not an afterthought.
When I started testing all of the recipes, the personal benefits were immediate and tangible. I had more regular, bulkier stools (a sign of optimal gut function). And I realized that all of the recipes I created for the prevention and maintenance phase aren’t just for people trying to prevent another flare-up. They’re recipes for anyone who wants to build adequate fiber into their daily routine without thinking about it constantly.
How Fiber Supports Blood Sugar and GLP-1 Signaling
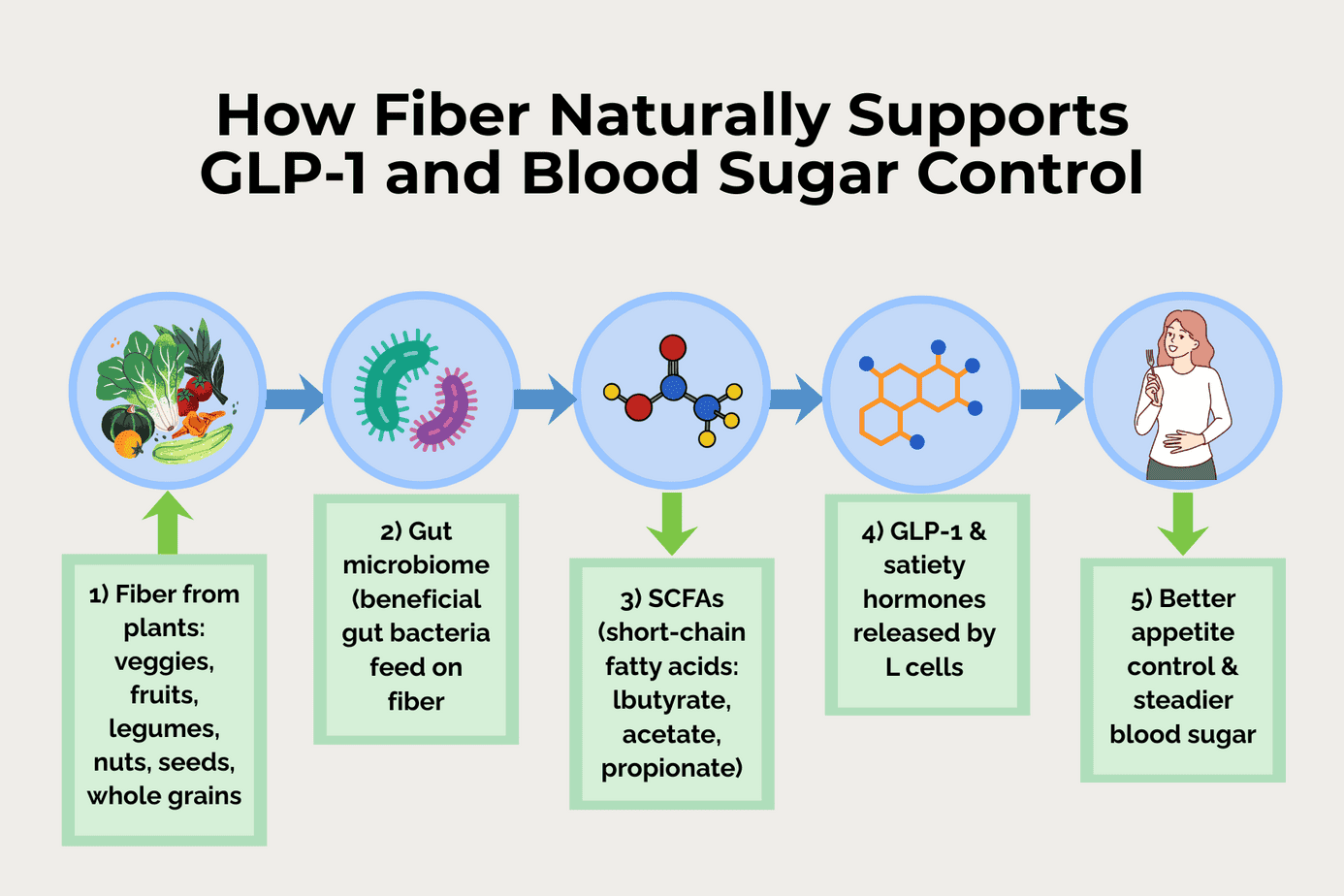
Dietary fiber does far more than “keep things moving.” Certain fibers directly influence how quickly glucose enters the bloodstream, how much insulin your body needs, and how much GLP‑1 your gut releases after a meal. Together, these effects smooth out blood sugar swings and support stable appetite signaling throughout the day. That means fewer crashes and cravings, and more predictable hunger.
Slows glucose absorption
When you eat refined carbohydrates alone, glucose rushes from your gut into your bloodstream, creating sharp rises and drops in blood sugar—often followed by rebound hunger.
Viscous, gel‑forming fibers change this. Found in foods like oats, legumes, chia seeds, flax, and low‑glycemic fruits, these fibers thicken the contents of your small intestine. This physically slows glucose absorption, blunting post‑meal spikes and reducing the demand on your pancreas to produce large insulin surges.
Triggers GLP‑1 release
Your intestine contains specialized cells called L‑cells that act like nutrient sensors. When you eat, they release satiety hormones including GLP‑1 and PYY (peptide YY, another fullness signal).
Here’s where it gets interesting: fermentable fibers that reach your colon intact become fuel for beneficial gut bacteria. These bacteria transform fiber into short‑chain fatty acids (SCFAs) like butyrate, propionate, and acetate, which are signaling molecules that talk directly to your gut and immune system.
Then, SCFAs stimulate L‑cells to secrete more GLP‑1. This enhances satiety, slows stomach emptying, and improves blood sugar handling—similar to GLP‑1 medications, but more gently and naturally.
Improves insulin sensitivity
Over time, eating more fiber improves insulin sensitivity. This means your cells respond more effectively to the insulin your body produces.
How? Researchers think this happens through several connected pathways, including:
-
- Reduced post‑meal glucose spikes
- Lower chronic inflammation
- A healthier gut microbiome
- Increased SCFA production
- Improved gut barrier function
All of these support more efficient insulin signaling. As a result, you experience steadier energy, fewer crashes between meals, and less of the urgent hunger that drives overeating and carb cravings.
How Fiber Feeds Your Gut Microbiome
Most of the fiber you eat never feeds you directly—it feeds the trillions of microbes in your colon. As they digest fiber, they generate signaling molecules that communicate with your gut, immune system, brain, and metabolic hormones, including GLP‑1. This is one of the main ways “just eating more fiber” quietly reshapes appetite, blood sugar, and inflammation.
SCFA production: butyrate, acetate, propionate
When gut bacteria ferment fiber, they produce short‑chain fatty acids (SCFAs) such as butyrate, acetate, and propionate. These SCFAs nourish colon cells, strengthen the gut barrier, and act like text messages from your microbiome to the rest of your body.
They help regulate inflammation, influence glucose production in the liver, and directly stimulate intestinal L‑cells to release GLP‑1 and other satiety hormones.
How gut bacteria amplify metabolic benefits
A well‑fed microbiome doesn’t just passively “live” in your gut. It actively helps manage your metabolism. Microbes that thrive on diverse fibers:
-
- Generate more SCFAs, which enhance GLP‑1 release, improve insulin sensitivity, and support more even blood sugar responses to meals
- Modulate the activity of appetite‑related hormones (like GLP‑1 and PYY) and stress‑related pathways that influence cravings and emotional eating
- Help calibrate how much energy you extract from food, nudging your system toward better metabolic efficiency rather than constant fat storage
In other words, the right microbes can take the benefits of fiber and multiply them—turning your gut into a hormone‑secreting, appetite‑regulating organ rather than just a digestion tube.
Microbiome diversity matters
Furthermore, not all microbiomes respond to fiber the same way. A diverse, resilient microbial ecosystem is more capable of producing a rich blend of SCFAs and beneficial signals than a depleted one.
Low‑fiber, ultra‑processed diets narrow that diversity. Varied plant foods—vegetables, fruits, legumes, nuts, seeds, and intact whole grains—encourage a broader, more robust microbial community.
Over time, that diversity helps maintain flexible, responsive GLP‑1 signaling, better blood sugar control, and a more stable relationship with food—even without medications.
Fiber’s Role in Metabolic Health and Detoxification
Fiber does more than support digestion and blood sugar. It helps your body eliminate compounds that interfere with metabolism and hormones. Think of fiber as your body’s cleanup crew, binding unwanted substances in the gut and escorting them out before they cause problems.
How fiber supports detoxification
Your liver works constantly to neutralize toxins, excess hormones, and environmental chemicals. Once processed, these compounds are packaged into bile and sent to your intestines for elimination.
Here’s the problem: without enough fiber, many of these substances can be reabsorbed back into your bloodstream instead of leaving your body. It’s like picking up your kids’ toys and putting them away, only to find them scattered all over the house again an hour later—they just keep recirculating.
Fiber changes this by:
-
- Binding bile acids, environmental toxins, and hormone breakdown products in your intestines
- Creating bulk that speeds transit through your digestive system
- Physically trapping compounds so they can’t be reabsorbed
- Moving waste efficiently into stool for elimination
Why this matters for weight and metabolism
Many modern chemicals act as “obesogens.” They push your body toward fat storage, insulin resistance, and hormonal imbalance, even in small amounts. Stored in fat tissue, they act as endocrine disruptors, interfering with the very hormones (like GLP-1) that regulate appetite and blood sugar.
Adequate fiber helps by:
-
- Supporting regular bowel movements (your primary elimination route for many toxins and hormone metabolites)
- Preventing hormone recycling (especially estrogen, which in excess can promote fat storage and symptoms of estrogen dominance)
- Gradually reducing your body’s overall toxic burden over time
- Supporting a healthier microbiome that can help transform and neutralize some of these compounds
The result is less background interference with the metabolic and hormonal systems that control weight, hunger, and blood sugar stability. Thus, consuming adequate fiber makes it easier for your body to respond to its own GLP-1 and insulin signaling.
“Food Noise” and the GLP-1 Connection
One reason GLP-1 medications have gained traction is their ability to quiet “food noise.” This is the constant mental chatter about food that drives obsessive thinking and eating beyond fullness. For many people on these medications, the realization is profound. They’re not thinking about food constantly anymore. They eat when hungry and stop when full. No mental battle. No white-knuckling through cravings.
Unfortunately, for many people, the food noise can return when they stop GLP-1 medications, the food noise can return. This is because the medication suppressed symptoms without addressing root causes.
When you address the root causes – gut health, blood sugar dysregulation, toxic burden, and missing nutrients – food noise quiets naturally. Not because you’re suppressing it, but because your body is finally functioning as designed.
We don’t lose weight to get healthy. We get healthy to lose weight.
GLP-1 drugs can quiet food noise chemically, but they don’t rebuild gut health, restore metabolic function, or establish the systems that support lasting change. Fiber helps do all of these things while supporting your body’s natural GLP-1 production:
-
- Increasing satiety (physical fullness signals)
- Feeding beneficial gut bacteria (that produce their own satiety signals)
- Stabilizing blood sugar (reducing hunger swings and cravings)
- Supporting detoxification (eliminating metabolic disruptors)
- Building gut barrier integrity (foundation for metabolic health)
Fiber doesn’t just quiet the noise temporarily. It helps rewire the relationship with food from the ground up, creating a system where healthy eating happens by default.
Building 25+ Grams of Fiber Into Your Day
Now let’s focus on getting you to 25+ grams of fiber per day consistently without obsessing over it.
Everyday foods that deliver real fiber
Only plant foods contain fiber—vegetables, fruits, legumes, nuts, seeds, and grains. Animal foods like meat, eggs, fish, and dairy have zero fiber. Therefore, diets like the Standard American Diet (heavy in processed foods and animal products), low-carb keto, and strict carnivore can leave people below their daily fiber needs.
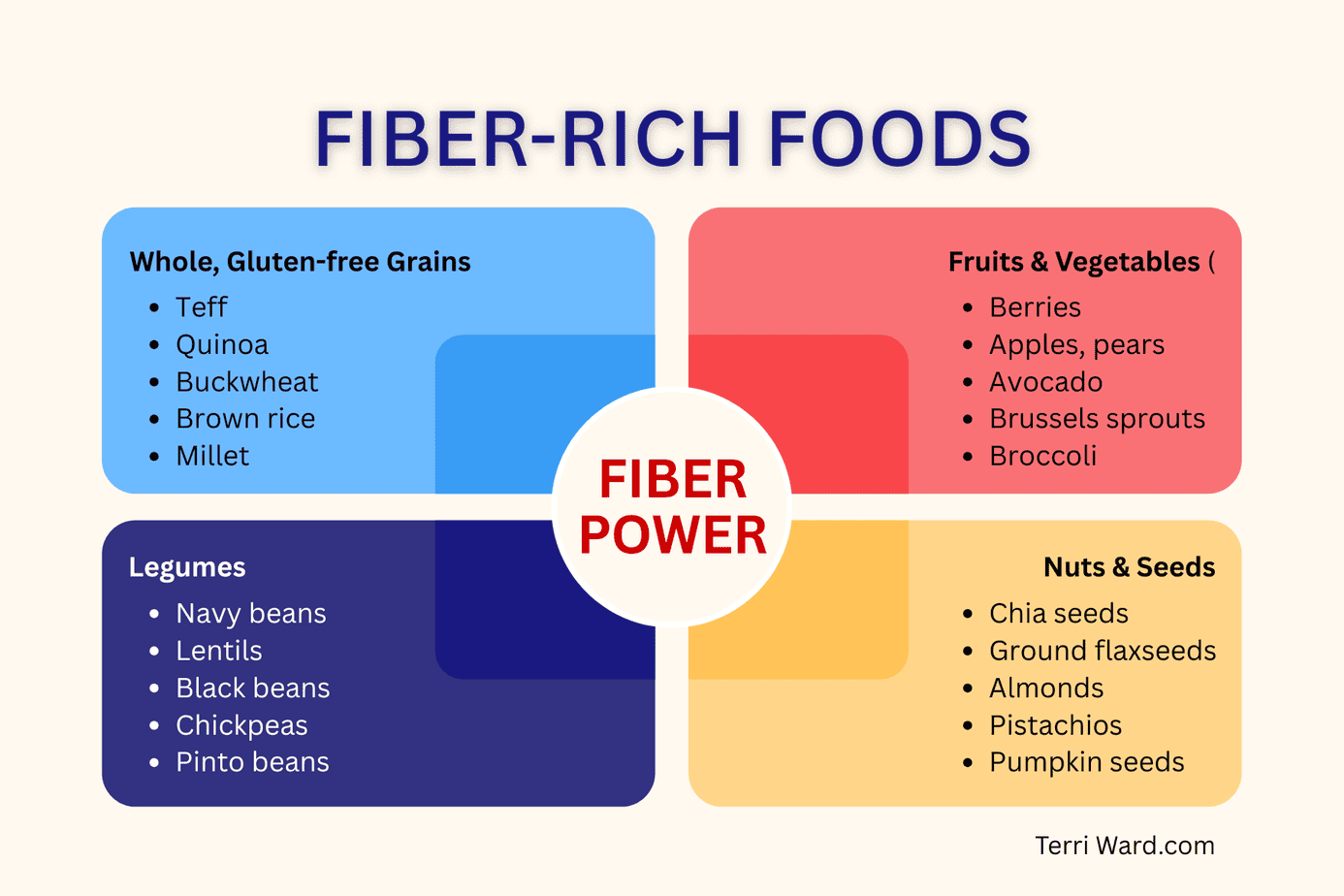
Some plant foods are especially helpful for blood sugar and GLP‑1 signaling. They provide a mix of soluble and insoluble fiber, and sometimes resistant starch. Examples include chia and flax seeds, legumes, intact gluten‑free whole grains, and avocado.
Quick Cheat Sheet of Fiber-Rich Foods
Most of your daily fiber can come from a few categories: whole gluten‑free grains, fruits and vegetables with skins, legumes, and nuts and seeds.
Tips for Boosting Fiber in Your Meals
-
- Whenever possible, choose whole gluten‑free grains (brown rice, quinoa, oats, millet) rather than foods made from white flours or starches.
- Leave edible skins on fruits and vegetables like carrots, potatoes, apples, delicata squash, etc. when you can to capture the extra fiber.
- Aim for at least 1/2 to 1 cup of legumes most days by adding beans or lentils to soups, salads, tacos, or grain bowls.
- Add 1 to 2 tablespoons of nuts or seeds (chia, flax, pumpkin seeds, almonds) to oatmeal, smoothies, salads, or roasted veggies to quietly raise fiber and satiety.
- Use avocado as a fiber‑rich, healthy fat—add slices to salads, grain bowls, tacos, or serve half an avocado with lime and salt as a simple, blood‑sugar‑friendly side or snack.
A Simple Daily Fiber Template
Instead of counting carbs and tracking every bite, you can use the Anti-Inflammatory Rainbow Diet (AIRD) plate as an easy visual for this. With each meal, aim for about half your plate from colorful non‑starchy vegetables. Divide the other half between lean protein and whole‑food starches like gluten‑free grains, legumes, or starchy vegetables. This naturally builds in fiber from multiple sources while keeping blood sugar steadier and avoiding a lot of math.
The template looks like this:
-
- 1 high-fiber breakfast anchor
- 1 fiber-heavy salad, soup, or bowl at lunch
- 2 fiber-rich snacks or snack-like add-ons
- 1 veggie-forward dinner with a whole grain or legume
Here are three different days built from this same template so you can see how flexible it is:
Day 1
-
- Breakfast (anchor): Chia pudding made with coconut milk, 2 to 3 tablespoons chia seeds, a handful of berries, a scoop of collagen peptides, and a scoop of clean protein powder. (NOTE: Always pre-soak chia seeds for at least 10 to 15 minutes before consuming. If eaten dry, they’ll pull moisture from your intestines, absorbing up to 12 times their weight in liquid and potentially causing discomfort and constipation.)
- Lunch (salad or bowl): Big salad with mixed greens, 3/4 to 1 cup black beans, 3 to 4 ounces grilled chicken, diced veggies, avocado, and olive oil vinaigrette
- Snack: Apple with 2 tablespoons almond butter
- Dinner: 4 to 6 ounces baked salmon with roasted Brussels sprouts and 1/2 to 1 cup quinoa tossed in olive oil or ghee
Day 2
-
- Breakfast: Gluten-free oatmeal (about 1/2 cup dry) cooked in milk of your choice with 1 scoop of collagen peptides and 1 scoop of protein mixed in, topped with 1 to 2 tablespoons ground flaxseed, 1/4 cup walnuts, and blueberries
- Lunch: Lentil and vegetable soup (at least 1 to 1.5 cups) with a side of mixed salad greens dressed in olive oil and vinegar of your choice
- Snack: Carrot sticks and bell pepper strips with 1/4 to 1/3 cup hummus
- Dinner: Stir-fry with 4 to 6 ounces chicken, broccoli and snap peas sautéed in avocado or olive oil, served over 3/4 to 1 cup cooked brown rice
Day 3
-
- Breakfast: Smoothie with spinach, berries, and 1 to 2 tablespoons chia or ground flax, 1/2 banana (optional) plus 1 scoop collagen peptides, 1 scoop clean protein powder, and 3/4 to 1 cup Greek or goat yogurt
- Lunch: Grain bowl with 1/2 to 1 cup quinoa or buckwheat, 1/2 to 3/4 cup chickpeas, roasted veggies, and tahini thinned with lemon juice and water to dressing consistency.
- Snack: Pear with ~1/4 cup shelled pistachios or pumpkin seeds
- Dinner: Baked potato or sweet potato (with skin), a generous serving of non-starchy veggies (e.g., broccoli, green beans, or a mixed veg medley), and 4 to 6 ounces of protein (salmon, chicken, or grass‑fed beef), with olive oil, butter, or ghee for fat
Notice how each day follows the AIRD plate pattern—half vegetables, plus protein and whole-food starch. This structure helps you hit your fiber target while supporting gut and immune health meal by meal. Once these “slots” are in place—your go-to fiber breakfast, default lunch bowl, standard snacks, and veggie-forward dinners—reaching 25 to 35 grams of fiber becomes automatic.
This is what a household system looks like.
You identify the meals and snacks that work for your family, keep the ingredients stocked, and rotate them regularly. Instead of making food decisions from scratch every day (which usually leads to convenience foods), you build a framework where better choices happen by default. You’re not following a restrictive diet—you’re shaping your environment to support fiber-rich eating.
It’s the same principle behind effective routines. When a pattern is built into daily life, it stops requiring constant motivation. Fiber intake shifts from something you “try” to do into something that naturally happens because your meals are structured to support it.
The Bigger Picture
Overall, fiber and blood sugar regulation are pieces of a larger puzzle. You can check out related posts here:
And in coming posts, I’ll explore how light pollution and toxins can disrupt metabolic health and contribute to weight gain.
If you’re struggling with blood sugar swings, constant cravings, or stubborn weight despite eating well, let’s talk. Inadequate fiber and poor gut health may be the missing pieces of your puzzle. Schedule a free 30-minute strategy session to discuss your symptoms and we’ll explore whether a root-cause approach could be your path forward.
Want more posts like this delivered to your inbox along with weekly Scripture, health news, and anti-inflammatory recipes?
Subscribe to the Wednesday’s Wisdom and Wellness newsletter below.
No spam. Unsubscribe anytime.